Posted in Itch Conditions.
- Article Teaser:
Psoriasis is a rare inflammatory disease that presents between the ages of 15 and 25, but can occur at any age. The body’s inflammation shows on the skin as pink plaques and scales. The condition can affect other organs as well, with 1 in 3 people with psoriasis developing psoriatic arthritis.

Psoriasis is a rare inflammatory disease that presents between the ages of 15 and 25, but can occur at any age. The body’s inflammation shows on the skin as pink plaques and scales. The condition can affect other organs as well, with 1 in 3 people with psoriasis developing psoriatic arthritis.
Psoriasis occurs in several different forms, each with its own unique features:
-
Chronic plaque psoriasis is the most common subtype, with rashes commonly affecting the elbows, knees, and the groove between the buttocks.
-
Guttate psoriasis is characterized by many small rashes less than 1 centimeter in diameter, usually involving the trunk and the upper segment of the arms and legs.
-
Pustular psoriasis shows up as small, pus-filled bumps and blisters. Patients with pustular psoriasis are likely to experience fever, chills, and malaise and are at higher risk of developing complications involving the kidneys, eyes, lungs, and liver.
-
Erythrodermic psoriasis involves a widespread rash that covers most of the body surface. The affected skin is usually painful, itchy, and may develop small pimple-like bumps.
What are the symptoms?
Psoriasis usually presents with red, itchy rashes that are sharply defined, ranging in size between 1 centimeters to more than 10 centimeters in diameter. Depending on the type of psoriasis, patients with psoriasis may also notice:
Psoriasis rashes usually affect the elbows, knees, trunk, and scalp, but can affect other parts of the body, such as the ear canals, the umbilicus (belly button), and palms and soles of the hands and feet. In certain types of psoriasis, the rash can involve most of the body surface. In children, rashes may occur on the face and scalp, in the diaper region, or on the sides of the arms and legs opposite the knees and elbows.
Common Questions
Is there a cure for psoriasis?
There is currently no treatment that completely cures psoriasis. Treatments for psoriasis are aimed toward reducing the severity of symptoms and minimizing their often debilitating impact on overall well-being. For more information on treating itch in psoriasis visit our treatment page
Where does psoriasis come from?
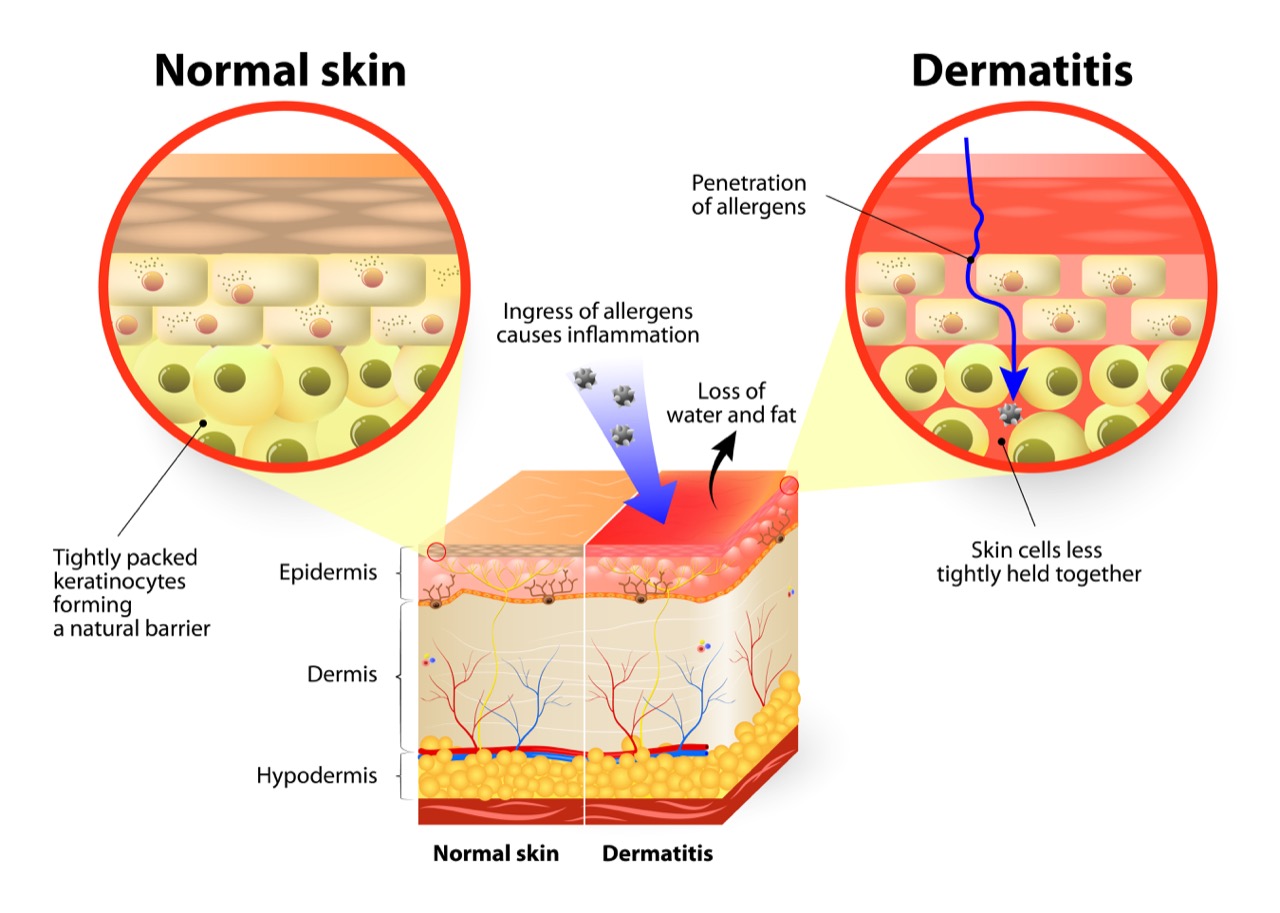
Psoriasis is a disease of the immune system that causes the outermost layer of the skin (epidermis) to grow rapidly. More specifically, it is believed that specific triggers cause immune cells to move to the epidermis, where they cause inflammation and release signals that cause skin cells to rapidly increase in number. While normal, healthy skin cells typically take about 4 weeks to mature and turn over, psoriasis patients’ skin cells do so within just a few days.
Who gets psoriasis?
Psoriasis can affect men and women of all ages. However, children are more likely to develop rashes that affect the scalp and diaper areas. Psoriasis is also commonly seen in individuals with HIV and is sometimes the first sign of infection.
Is psoriasis contagious?
Psoriasis is not an infectious disease; therefore, it is not contagious and cannot be passed from one person to another.
How is psoriasis diagnosed?
Physicians can diagnose psoriasis based on a thorough skin examination and a close evaluation of your medical and family history. If you think you may have psoriasis, please contact a dermatologist for further evaluation.
Psoriasis
Read more …What is Psoriasis?